- Home
- Billionaires
- Investing Newsletters
- 193CC 1000
- Article Layout 2
- Article Layout 3
- Article Layout 4
- Article Layout 5
- Article Layout 6
- Article Layout 7
- Article Layout 8
- Article Layout 9
- Article Layout 10
- Article Layout 11
- Article Layout 12
- Article Layout 13
- Article Layout 14
- Article Sidebar
- Post Format
- pages
- Archive Layouts
- Post Gallery
- Post Video Background
- Post Review
- Sponsored Post
- Leadership
- Business
- Money
- Small Business
- Innovation
- Shop
Recent Posts
German Man Likely Cured of HIV, Researchers Say
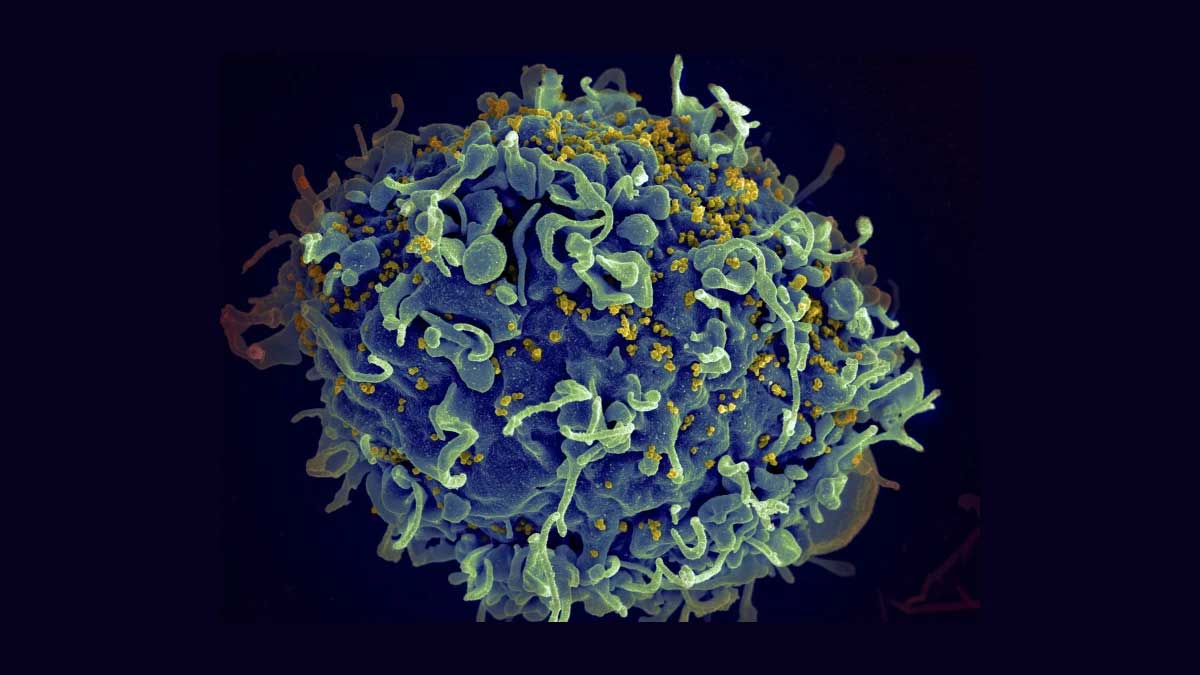
In a significant breakthrough, researchers have announced that a German man appears to be the seventh person in history to be cured of HIV. This development follows a pioneering stem cell transplant he received nearly a decade ago. The patient, who has been described as the “next Berlin patient” in reference to the first individual cured of HIV, underwent this revolutionary treatment in 2015 to address his leukemia. Since then, he has maintained remission from HIV after discontinuing antiretroviral therapy in late 2018. This case stands out as it involves a unique approach to HIV treatment, where the stem cell donor had a rare single mutation resistant to HIV, marking a departure from previous cases where double mutations were involved.
Dr. Christian Gaebler, a leading researcher on this case, emphasized the significance of this single mutation. This genetic variation alters a crucial protein that HIV uses to enter human blood cells, rendering it less effective at infecting individuals with this mutation. The fact that the virus can still infect people with this mutation but progresses much more slowly in the absence of antiretroviral drugs offers promising implications for future HIV cure strategies. This new finding suggests that expanding the criteria for selecting stem cell donors to include those with this single mutation could potentially enhance the success rate of similar treatments, making them more accessible to a broader patient population.
The historical context of HIV cure research highlights several notable successes prior to this case. The first significant breakthrough occurred in 2009 with Timothy Ray Brown, known as the “Berlin patient,” who was reported to have been cured of HIV following a stem cell transplant from a donor with a double HIV-resistant mutation. This milestone was followed by similar reports of success involving the “London patient” and the “City of Hope” patient, as well as the “New York” patient, who were all considered cured by 2022. In the previous year, the “Geneva patient” and the “Düsseldorf patient” were also reported to have achieved remission from HIV. All these patients underwent stem cell transplants primarily aimed at treating blood cancers and received cells from donors with HIV-resistant mutations, underscoring the role of these genetic variations in successful treatment outcomes.
The global impact of HIV remains profound, with the World Health Organization estimating that approximately 39 million people worldwide were living with HIV by the end of 2022. During the same year, around 630,000 individuals succumbed to HIV-related illnesses, highlighting the persistent challenge of managing and ultimately curing the virus.
Currently, there is no universally effective cure for HIV, a virus known for its ability to undermine the body’s immune system. The Centers for Disease Control and Prevention (CDC) indicate that once an individual contracts HIV, it remains in the body for life. Despite advances in treatment, including the use of stem cell transplants and anti-HIV genes or mutations, HIV often progresses to AIDS (acquired immunodeficiency syndrome) if left untreated. Initial symptoms of HIV infection, which can resemble flu-like conditions, typically manifest within two to four weeks, though definitive diagnosis requires specific testing.
This latest development in Germany not only represents a hopeful advancement in HIV cure research but also suggests a potential shift in treatment approaches. The identification of effective single mutations in stem cell donors could pave the way for more inclusive and effective treatment options, offering renewed hope for those living with HIV worldwide.
Recent Posts
Categories
- 193cc Digital Assets2
- 5G1
- Aerospace & Defense46
- AI37
- Arts3
- Banking & Insurance11
- Big Data3
- Billionaires462
- Boats & Planes1
- Business328
- Careers13
- Cars & Bikes76
- CEO Network1
- CFO Network17
- CHRO Network1
- CIO Network1
- Cloud10
- CMO Network18
- Commercial Real Estate7
- Consultant1
- Consumer Tech180
- CxO1
- Cybersecurity68
- Dining1
- Diversity, Equity & Inclusion4
- Education7
- Energy8
- Enterprise Tech29
- Events11
- Fintech1
- Food & Drink2
- Franchises1
- Freelance1
- Future Of Work2
- Games141
- GIG1
- Healthcare78
- Hollywood & Entertainment186
- Houses1
- Innovation42
- Investing2
- Investing Newsletters4
- Leadership65
- Lifestyle11
- Manufacturing1
- Markets20
- Media193
- Mobile phone1
- Money13
- Personal Finance2
- Policy567
- Real Estate1
- Research6
- Retail1
- Retirement1
- Small Business1
- SportsMoney33
- Style & Beauty1
- Success Income1
- Taxes2
- Travel10
- Uncategorized8
- Vices1
- Watches & Jewelry2
- world's billionaires431
Related Articles
What Healthcare Can Learn from Nvidia’s Success
The tech industry is undergoing a seismic transformation, with two of its...
By 193cc Agency CouncilDecember 16, 2024Salmonella Triggers Recalls of Costco Eggs and Cucumbers
The recent salmonella outbreak has prompted the recall of two major food...
By 193cc Agency CouncilNovember 30, 2024Bird Flu Found in Raw Milk in California, Recall Issued
California health authorities have confirmed the presence of the bird flu virus...
By 193cc Agency CouncilNovember 25, 2024UniDoc Health Launches Mobile ‘Health Cube’ for Remote Care
UniDoc Health, a Vancouver-based company, is revolutionizing healthcare accessibility with the launch...
By 193cc Agency CouncilNovember 23, 2024














Leave a comment